OMM in the OR: Division of Surgical Oncology Faculty and Resident Team Awarded the First TOMF-Funded Research Grant

The Department of Surgery at the University of Arizona College of Medicine – Tucson is proud to announce that general surgery resident Ivy Stejskal, DO, has been awarded a $5,000 research grant from the Tucson Osteopathic Medical Foundation (TOMF)—the foundation’s first-ever grant dedicated to sponsoring research.
This award was created after TOMF learned about Dr. Stejskal’s IRB-approved study, “The Impact of Osteopathic Manipulative Medicine on Radiotracer and Isosulfan Blue Dye Uptake During Breast Conserving Surgery and Sentinel Lymph Node Biopsy (SLNB).” The project drew the attention of Franz Rischard, DO, Director of the Pulmonary Hypertension Program in the Division of Pulmonary, Critical Care, and Sleep Medicine at the University of Arizona, who served on the IRB committee reviewing the study. Once the study was approved, Dr. Rischard was impressed by the innovative approach and sought to help secure funding through TOMF to launch the research. Recognizing the significance of this work, TOMF established a new research funding program for DO investigators, selecting Dr. Stejskal as its inaugural recipient this past summer.

Dr. Stejskal began the study with the first enrolled patient on July 1, 2025, under the mentorship of Nova Foster, MD, FACS, Clinical Professor of Surgery and Medical Director of the Breast Program at Banner – University Medical Center Tucson and the University of Arizona Cancer Center, as well as Jad M. Abdelsattar, MD, Breast Surgical Oncologist and Clinical Assistant Professor of Surgery, and Jennifer Erdrich, MD, MPH, MFA, FACS, FSSO, Assistant Professor of Surgery. The surgical oncology team has already enrolled 15 patients, with a goal of reaching 30 participants in phase one.
Reflecting on what it means to receive the foundation’s first-ever grant supporting OMM-related research, Dr. Stejskal shared:
“It’s very exciting to receive the first award because it means the foundation can use our study as a building block for even more grants in the future. While the division of surgical oncology participates in extensive research projects, the breast department does not currently have a designated, funded lab. This grant gives us the opportunity to have that additional financial support.”
What is a Sentinel Lymph Node Biopsy (SLNB)?
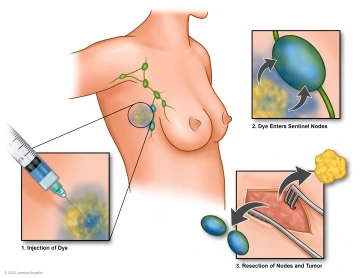
For patients diagnosed with breast cancer, SLNB is a surgical procedure to identify and remove the sentinel lymph node(s)—the first nodes likely to receive metastatic cancer cells from the tumor. This step helps determine the cancer stage and guides treatment planning.
Under current practice, radiotracers and blue dye are injected near the tumor once the patient is sedated. A five-minute breast massage helps move these markers to the axillary lymph nodes, where surgeons then locate and remove affected nodes. However, uptake of these tracers can be inconsistent, sometimes requiring more extensive dissection.
How Osteopathic Manipulation Could Help
Dr. Stejskal’s study explores whether osteopathic manipulative medicine (OMM) can improve lymphatic flow and tracer uptake. In addition to the standard five minutes of massage, the experimental group receives four more minutes of targeted OMM techniques, including a combination of:
- Thoracic Inlet and Outlet: Steering Wheel Technique
- Pectoral Traction targeting the Pectoralis Major, Pectoralis Minor, and Anterior Deltoid
- Anterior Thoracic (Lymphatic) Pump
- Lateral Thoracic (Lymphatic) Pump
Patient Participation
Eligible patients undergoing breast-conserving surgery (lumpectomy) at the clinics of Drs. Foster, Erdrich, and Abdelsattar are screened in advance and must meet criteria, including:
- No evidence of metastatic disease
- No prior breast surgery
- Able to tolerate full shoulder range of motion
Participants are randomized to either the standard five-minute massage or the enhanced OMM protocol. Overall, the additional time under anesthesia is minimal, and risks remain low.
The Inspiration Behind the Research
During her intern year on the surgical oncology service, Dr. Stejskal discussed her osteopathic background and training with Dr. Foster. Dr. Foster recalled a previous DO resident who used OMM during an SLNB case and noted what seemed to be improved tracer uptake, though no formal study followed. Recognizing an opportunity for innovation, Drs. Foster and Stejskal began an 18-month process of IRB review and approval to launch the research.
Throughout the research development process, Dr. Stejskal sought guidance from both current and former mentors, including Michael Ditillo, DO, FACS, program director of the University of Arizona General Surgery Residency and clinical associate professor of surgery in the Division of Trauma, Critical Care, Burns and Emergency Surgery, and Jennifer Ribar, DO, from Pacific Northwest University of Health Sciences, where Dr. Stejskal completed her medical training. Their expertise and insight were instrumental in refining the study’s approach, ultimately helping to identify the four optimal OMM techniques for this procedure.
Looking back on her path to this launching this research study, Dr. Stejskal reflected:
“When I first rotated through the breast surgical oncology service, I truly found the surgical specialty I wanted to pursue—you get valuable experience in the clinic, can build long-term patient relationships, and also get a good amount of OR time. Breast cancer patients and their support networks are an incredible and resilient group of people, and I am excited to be able to continue to train and do research so I can serve them to the best of my ability in the future.”
Impact of the TOMF Grant
The TOMF grant will support data collection, statisticians, publications, and enable Dr. Stejskal to present the team’s findings nationally. She anticipates sharing preliminary results at the Society of Surgical Oncology and American Society of Breast Surgeons meetings this spring. The project is already attracting attention, with Dr. Stejskal invited to speak next month at the American College of Osteopathic Surgeons Annual Clinical Assembly in Salt Lake City, Utah, on the role of OMM in the operating room and its impact.





