After Deep Brain Stimulation Surgery, Tucson Mom with Parkinson's Finds Joy in Simple Things

The tremors and stiffness that prevented Maureen Raine from doing so much of what she loved have all but disappeared after she underwent deep brain stimulation surgery or DBS in July.
The surgery was performed by Willard S. Kasoff, MD, MPH, a University of Arizona neurosurgeon and director of the Neuromodulation Program in the UA Department of Surgery.
Raine, who suffers from a young-onset form of Parkinson's disease, first began having difficulty using her right side due to tremors and stiffness. Diagnosed at age 37, her disease was progressing quickly, and she relied on high doses of medication in an attempt to control symptoms. The frequent dosing and side effects of her medication, called Levodopa, interrupted her days and began to take over her life.
Now, on most days, Raine forgets she has Parkinson's disease.
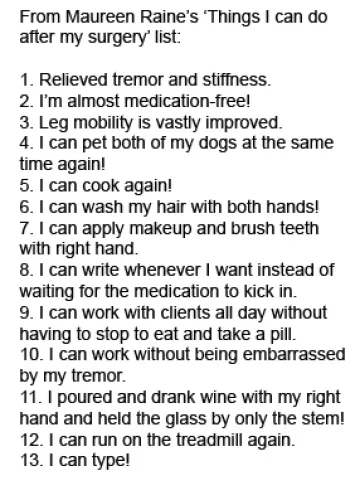
What is amazing is all of the joyful things I got back said this 40-year-old Tucson personal trainer, who keeps a growing list of Things I Can Do After My Surgery (See box.)
On the list is cooking, petting her dogs, washing her hair with both hands, running pain-free and writing again whenever she wishes without having to wait for medication to kick in.
Since the surgery, she has checked a few things off her bucket list including riding a mechanical bull and zipping around town on her motorcycle.
I have my physical capabilities back Raine said. The surgery was a piece of cake
DBS is a surgical procedure used to treat disabling neurological symptoms, most commonly the debilitating motor symptoms of Parkinson's disease that include tremor, rigidity, stiffness, slowed movement and problems with walking. Other conditions that can be treated include essential (or benign) tremor, primary dystonia and severe cases of Tourette's syndrome or obsessive-compulsive disorder.
While DBS is not new, not enough patients with Parkinson's and other movement disorders currently benefit from the procedure, Dr. Kasoff said. It is so underperformed that for many people it is a novel idea, even though it has been well-established for more than 20 years he said.

Dr. Kasoff, who joined the UA Department of Surgery in 2014, expects to perform about 25 procedures this year.
In many cases, DBS produces an immediate effect, and it can be a dramatic effect Dr. Kasoff said. It can provide a huge benefit to patients quality of life. It enables people to regain a level of function that the disease has taken away. It can allow people to enjoy their lives longer while living with a disease that at the moment we dont have a cure for
Raine's UA neurologist, Sudeshna Bose, MD, an assistant professor in the Department of Neurology, suggested that she explore deep brain stimulation and she met with Dr. Kasoff. While Raine was nervous at the thought of brain surgery, she was comforted by the low risks associated with the highly successful treatment option.
I was scared to death, but I did my research she said.
And she was confident in Dr. Kasoff and the Banner University Medical Center Tucson team.
Dr. Kasoff was amazing and the hospital provided wonderful care Raine said.
Dr. Kasoff said DBS is an extremely well-established, safe surgery, and while there are risks with any surgery, the risks in this case are extremely low
Since her symptoms were only on her right side, surgery was performed on the left side of her brain. Patients often are awake for portions of the procedure, but options are available for patients who prefer not to be awake, Dr. Kasoff said.
During the procedure, the patient's head is held in place with a rigid frame and an incision about 2 inches wide is made behind the hairline. A hole the size of a dime is made in the skull to allow the neurosurgeon and neurologist to map the target brain structure and place the DBS electrode in the precise location to best control the patient's symptoms. During a second surgery, a small, battery-powered computer is implanted near the collarbone, similar to a cardiac pacemaker.

These devices sometimes are called brain pacemakers since they normalize the abnormal brain patterns of patients with Parkinson's disease or tremor said Dr. Kasoff, adding that battery replacements are usually made every five to seven years in a minor, outpatient procedure.
During surgery, Raine felt her right foot and hand, which she called gnarled relax. She spent one night in the hospital and was running errands within a couple of days.
One of the advantages of deep brain stimulation is it mimics the effect of medications for Parkinson's disease without the side effects and in a more controlled manner Dr. Kasoff said. DBS is not a cure, and we all are working toward and hoping for a cure; but until we have that cure, DBS is our best treatment for symptom control.
The wonderful thing about DBS is that it helps people live better lives right now, but does not prevent someone from taking advantage of future therapies either Dr. Kasoff added.
Most Parkinson's patients are either candidates now or at some point in their illness will become candidates, he noted. It's most important that patients be seen by a neurologist who specializes in movement disorders. Not all symptoms will respond, not everyone is a candidate and every patient requires an individualized treatment plan with an expert multidisciplinary team
DBS has an interesting history, tracing back to lesioning procedures developed in the 1950s and 1960s, when it was discovered that small holes could be burned in areas of the brain to relieve tremors. What was discovered in the late 1980s and developed during the 1990s is that electrical stimulation could have the same effects, but it is safer, adjustable and reversible Dr. Kasoff said.
A relatively small group of neurosurgeons perform the procedure, which currently is in a golden age of rapid progress and transformation, he said. There are tens of thousands of patients who likely would benefit from DBS, but either dont know about it or have other barriers such as lack of access to specialty care.
He said patients benefit when the procedure is performed at academic medical centers like BUMCT, with collaboration among neurosurgery, neurology and neuropsychology. In addition to Drs. Kasoff and Bose, the multidisciplinary team at BUMCT also includes neurologists Scott Sherman, MD, PhD, UA associate professor and director of the Movement Disorders Center of the UA Department of Neurology; Hong Lei, MD, PhD, UA assistant professor and director of the Department of Neurology's Acupuncture Service; and Tanya Lin, MD, UA assistant professor of neurology; and Marisa Menchola, PhD, UA assistant professor of neurology and psychiatry. In addition, research partnerships are under way with the University of Arizona Center on Aging and other groups at the UA to study the effects of DBS on gait and balance.
Following surgery, Raine is performing at top level on the job, working with clients who have physical challenges.
I am not 100 percent, but I am pretty darn close she said. My son says I am part robot. We have fun with it
Dr. Kasoff said Raine's outcome is typical. Maureen had a wonderful and very gratifying response although not an unusual one. That's why it is such a rewarding procedure to perform because outcomes like hers are quite common. I get a kick out of her energy and the way she has dived right back into her life
Raine is enjoying the freedom to hike, run and have fun with her kids, son Sean, 17, and daughter Katelyn, 15.
They think Im a super hero she said. This was life-changing, and I would do it again in a second
Since the DBS surgery, Raine has checked a few things off her bucket list including riding a mechanical bull, as shown in this video.

