Breast Reduction:
People with disproportionately large breasts may experience physical discomfort like upper back or neck pain and skin irritation, and they may find it more challenging to do everyday activities or exercise. Additionally, for some, disproportionately large breasts may lead to self-consciousness or attract unwanted attention. Breast reduction, or reduction mammoplasty, makes large breasts smaller. There are a variety of reasons why someone may want to pursue breast reduction, and ultimately the decision lies with the individual determining what is best for them.
What does a breast reduction involve?
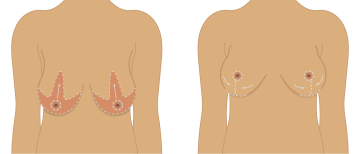
A breast reduction includes the removal of fat, glandular tissue and skin. There are two common methods of breast reduction: the “keyhole” (aka “inverted T”) method and the free nipple graft.
Keyhole Method
The keyhole, or the inverted T method, is more likely to retain breast sensation and the ability to breastfeed. This is because in this method, the nipple and areola remain connected to the breast tissue, blood vessels, and nerves during the procedure.
Free Nipple Graft Method
The free nipple graft method is used when such a large volume to breast tissue is being removed that it places the nipple at risk for not surviving. In these cases, the new breast mound is created, then the nipple areolar complex is grafted, much like a skin graft, on the new breast mound in an anatomic position. In this case, the nipple does not have sensation.
Breast Reduction Frequently Asked Questions
Following a breast reduction, in most cases, scarring is hidden in the crease under the breasts and along the edge of the areola, and often those scars will fade into light lines.
Similarly, in most cases, the nipple and areola will be moved higher on the breast, and if appropriate, a surgeon may be able to make the areola smaller.
Breast shape and size differs based on many factors, like any future pregnancies, menopause, and weight fluctuations. While no two breasts are perfectly identical, a breast reduction can help even out two significantly differently-sized breasts. During a breast reduction, a surgeon can also reshape the breasts to be positioned higher.
The sensitivity of breasts tends to change following a reduction. Usually there is less sensation in the first year after a reduction. In rare occasions, breasts can become extra sensitive. Over time, the numbness or sensitivity may return closer to normal, though some change may be permanent.
A breast reduction surgery often includes the removal of some milk glands or ducts, possibly preventing breastfeeding in the future. In general about 2/3 of women who have had breast reductions have been able to subsequently breast feed. That does mean the 1/3 cannot. Be sure to speak with your surgeon if this is important to you.
Sometimes, when a breast reduction is performed with the goal of reducing significant pain or addressing very specific insurance designated medical problems, insurance will cover the surgery. Anyone looking into pursuing a breast reduction should speak with their insurance company about their options and criteria for insurance coverage.
Prior to the surgery
Anyone interested exploring breast reduction surgery will meet with a program intake provider for an initial consultation to answer any questions you might have, discuss goals for the surgery, mitigate any risks you have associated with surgery, and identify a surgery plan. The consultation also includes a physical exam and a discussion about your health history. Please bring a list of your current medications, including:
- Prescriptions
- Birth control medicines
- Over-the-counter medicines (includes allergy pills, cough medicine, etc.)
- Inhalers
- Patches
- Vitamins, supplements, or herbal remedies.
Following the initial consultation, if you have decided to pursue a breast reduction, are deemed low risk for complications, and meet insurance coverage requirements, you’ll meet with the surgeon to discuss your surgery.
During the surgery
Breast reduction surgeries typically take about 4 hours. During the surgery, based on the surgery plan and method, the surgeon will mark each breasts. Patients will receive general anesthesia and recommended regional “blocks,” which is numbing medicine for the chest to reduce pain immediately following surgery. The surgeon will then make incisions along the markings to remove extra fat, breast tissue, and skin. The nipple and areola are moved higher on the breast, and the rest of the skin is brought in around the areola to form the smaller breast. To conclude, incisions are closed with stitches, and breasts will then be wrapped in bandages and a surgical bra.
After the surgery
Please bring someone with you to the hospital and prepare for someone to help care for you during the first few days following your surgery. Recovery typically takes a week or two at your home. You may be given pain medicine like acetaminophen (Tylenol), ibuprofen (Advil), and limited prescription-grade narcotic medication for any breakthrough pain. Your breasts will likely be swollen and bruised for the first week, but over the next three months they will eventually settle to their final size and shape. As your incisions heal, scarring is most prominent for the first 9-12 months after surgery. Over this time, they usually fade to light lines.
Like with any surgery, complications associated with breast reduction surgery are possible, and understanding the risks are an important component of coming to an educated, informed decision about whether breast reduction surgery is right for you.
Although rare, complications from breast reduction surgery are still possible. Please share with your doctor any questions or concerns you have related to these risks.
The risks of surgery can be higher if you are in poor health. You must obtain a medical release from your primary care doctor to have breast reduction surgery if you have a serious medical condition. If you are a smoker, either tobacco or marijuana, you are not a candidate for surgery until you have stopped all smoking for 6 weeks prior to any planned surgery. If you have diabetes or high blood pressure, these must be treated by you primary care team and have normalized prior to any surgery. In addition to these, many other health factors may contribute to complications after a breast reduction. It is for this reason it is important to have a medical release by your primary care provide prior to any surgery.
Let your surgeon know if you have had an allergic reaction in the past to any medications, latex, or other substances as well as if you have had any prior issues with anesthesia.
Potential risks and complications for any surgery include:
- Reactions to anesthesia or medications. Although most are not serious, some reactions can be dangerous, and even deadly. Your medical team is trained in case a serious allergic reaction does happen.
- Bleeding after surgery. There is a possibility you will start bleeding after surgery. In rare cases, a follow-up operation may be needed to stop the bleeding.
- Blood clots. The risk of blood clots forming in either one or both legs during your procedure is small, but in very rare cases, a clot can travel to the heart or lungs and cause serious complications.
- Infection. The medical team will work to prevent infection, but in rare cases one can still develop.
Potential risks and complications for breast surgery:
- Changes in breast feeling and/or function. This may include numbness of the breasts or increased sensitivity in nipples or breasts.
- Different results than expected. This may include continued back or neck pain from other causes or breast size and shape differences.
- Healing problems. This may include wounds that are not healing properly, or reopening of wounds, though this is uncommon.
- Inability to breastfeed. If you are considering breast reduction surgery but would like to be able to breastfeed in the future, be sure to share that priority with your health care providers.
- Skin around scars blackens or becomes blistered. There is a small chance of this happening, but it occurs more often among smokers or those with an infection. This may have to be treated with surgery.
How do I decide?
Making a decision this big is understandably difficult. If you are unsure whether to proceed with breast reduction, try exploring these discussions:
- Upper back (between shoulder blades) or neck pain caused by the weight of large breasts
- Grooves on shoulder from your bra straps that are bothering you
- Rashes or other skin problems caused by breast size
- Difficulty exercising or being as active as you would like due to breast size
- Facing unwanted attention or you are self-conscious about your breasts
- Unable to wear the clothes you like due to your breast size
- You are at your insurance designated age (generally must be older than age 18)
- You have the documented insurance requirements
- You are not overweight (generally as close to or less than a BMI of 30)
- Worried about the potential risk of the surgery
- You don’t want scars
- Breast sensitivity is important for you
- Want to be able to breastfeed
- Worried about your insurance not covering the surgery
- Overweight (greater than a BMI of 32)
- Too young (less than age 16)
- Unable to provide documented insurance requirements
Consider your goals of the surgery that are most important to you. Look at the decision factors section to help with your decision.
Talk with an intake provider. An initial consultation is not a commitment to surgery, and speaking with a breast reduction specialist can help give you clarity regarding the plan for the surgery, options available to you, and anything that may concern you about the surgery.
Talk with those who love and support you. Your friends and family may have valuable insights and perspectives and can help you navigate the decision making process.
Make an Appointment
For the best plastic and reconstructive surgical care in Tucson, Southern Arizona or the Southwest, make an appointment by calling
(520) 694-8888.
Contact Us
University of Arizona Department of Surgery
Section of Plastic and Reconstructive Surgery
1501 N. Campbell Ave.
Tucson, Arizona 85724
Office Phone: (520) 626-9383
Fax: (520) 441-4945